Generally speaking, fewer women smoke than men. There are however, cultural and regional variations and greater gender differences are found in South Korea, Indonesia, and China, compared to Europe and the United States. South Korea, for instance, has the highest male smoking rate and the lowest female smoking rate of all (OECD) countries (Park et al., 2014). The World Health Organization (2017) estimates that 40% to 50% of men and 4% to 8% of women in Korea smoke; according to the OECD (2015) it is 31.3& of males and 3.4% of females (Gunter et al., 2020). Gender is a factor.

Women may encounter negative social attitudes toward women's smoking. This stigma can have an impact on their smoking cessation motivation and concealment (David et al., 2024). Korean women, for instance, underreport their smoking activity because of the stigmatisation. This stigma may prevent many Korean woman from smoking (Woo, 2018). Using biological indicators (urinary cotitine concentration), others come to the conclusion that the "actual female smoking rate is significantly highere than official records state" and that the social desirability bias produces results that underestimate the number of female smokers (Park et al., 2014).
This study shows that the actual female smoking rate is significantly higher than that reported officially, but also that the gap is decreasing steadily. Females exhibited a higher rate of false responses, which resulted in an underestimation of the female smoking rate. (Park et al., 2014)
Concealment is not really surprising given harsh reactions might be possible as the following two anecdotes imply:
"I was a bit tipsy and felt like a puff. After I lit the cigarette, a random middle-aged man came up to me and started shouting as if I had done something very bad. He said, ‘I will slap your face if you don't throw your cigarette away right now.' He called me ‘dirty little woman.'" (Kim, 26)
"When I was smoking outside, an old man shouted at me how dare I, a female, smoke there. People say the social atmosphere about female smoking has changed but this kind of thing still happens. Men cannot understand how scared women get in those situations." (Lee, 33)
In South Korea, women use heated tobacco products for different reasons than men do, i.e., to avoid the stimga associated with female smoking while men use them to avoid family members putting pressure on them to stop smoking (Kwanwook et al., 2020)
As has been well-established by previous studies, the smell of cigarettes was the main reason for using HTP for both male and female users. Nevertheless, there was a gender difference in the cause for concern about the smell of cigarettes, especially regarding the person(s) to whom participants thought the smell was an issue. Males tended to identify smell as a problem when it came to their familial responsibilities with their wives and children. Many participants felt guilty for using cigarettes due to their harmfulness to health and exposing their family members to secondhand smoke. For these participants, these feelings, usually recognised, and revived by the very smell of tobacco, could be reduced through the use of HTPs with a relatively low odour. Therefore, males were more concerned with the ‘physical’ characteristics of the cigarette smell as a reminder of the harmfulness of tobacco.
‘When I got married, my wife knew that I was a smoker and did not care too much. But when she got pregnant, she kept telling me, “Your body smells of cigarettes. Don’t come near, it’s bad for a child”. She told me a lot to stop smoking. So, I thought about various ways, and finally bought IQOS which was easily available. I think it would be better to choose one that doesn’t smell to my family.’ (Male, 39 years)
Unlike the male participants, female participants were more interested in the ‘socio-cultural’ rather than physical characteristics of the tobacco smell. In other words, women were conscious that their tobacco smell would expose their smoking habit in a patriarchal society where female smoking is still a highly stigmatised activity, particularly in the workplace. Therefore, unlike men, they were reluctant to disclose their smoking habit. In particular, women with children were extremely vigilant about concealing such socially unacceptable behaviour as smoking, when among other parents and their children’s teachers, because of the perception that they should be a morally upright ‘agi-eomma’ (a baby’s mother). For these reasons, women chose HTPs to maintain their social status as a righteous working woman or mother.
‘I should not let my colleagues in the company notice the smell from my smoking. Since my sister introduced me to “lil”, I have used it while working and smoked CCs at home.’ (Female, 22 years)
‘For me, [the] IQOS has solved every interpersonal problem caused by the smelly cigarette. Now I have been able to avoid uncomfortable gazes, [I am] liberated from the smell, and [I have] improved interpersonal relationships with my children’s teachers or other parents. I used to be unable to smoke openly because I was given kind of a name tag called “agi-eomma” (a baby’s mother).’ (Female, 42 years) (Kwanwook et al., 2020)
- - - - - - - - - - - - - - - - - -
- David, J.-C., Fonte, D., Sutter-Dallary, A.-L., Auriacombe, M., Serre, F., Rascle, N. & Loyal, D. (2024). The stigma of smoking among women: A systematic review. Social Sciene & Medicine, 340, 116-491. Korean Journal of Family Medicine, 41(3)
- Gunter, R., Szeto, E., Jeong, S.-H., Suh, S. & Waters, A. J. (2020). Cigarette Smoking in South Korea: A Narrative Review.
- Kwanwook Kim,
Jinyoung Kim,
Hong-Jun Cho (2020). Gendered factors for heated tobacco product use: Focus group interviews with Korean adults. Tobacco Induced Diseases, 18(43), link
- Myung Bae Park, Chun-Bae Kim,corresponding author Eun Woo Nam & Kyeong Soo Hong (2014). Does South Korea have hidden female smokers: discrepancies in smoking rates between self-reports and urinary cotinine level. BMC Womens Health, 14(156), link
- Woo, C. (2018). Gendered Stigma Management among Young Adult Women Smokers in South Korea. Sociological Perspectives, 61(3), link
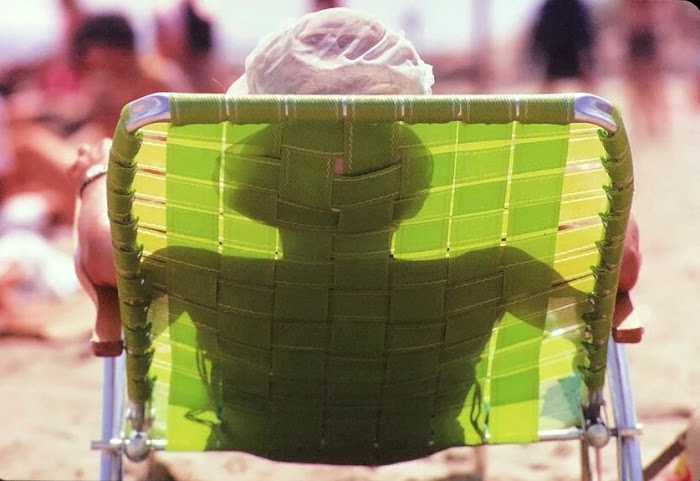
- photograph by Nina Ahn via







































 x
x